Subject’s age: 19
Subject’s gender: Female
Reason for visit:
- Bilateral hip/knee pain. Patient has history of bilateral hip/knee pain. She has recently increased training intensity with running. She is able to run 1 mile before onset of pain. Patient reports that pain has steadily increased. Patient is currently unable to run without bilateral leg pain.
- Patient medical history is consistent with hypermobility syndrome. Patient has a 8/9 score with Beighton mobility assessment.
Noraxon hardware used:
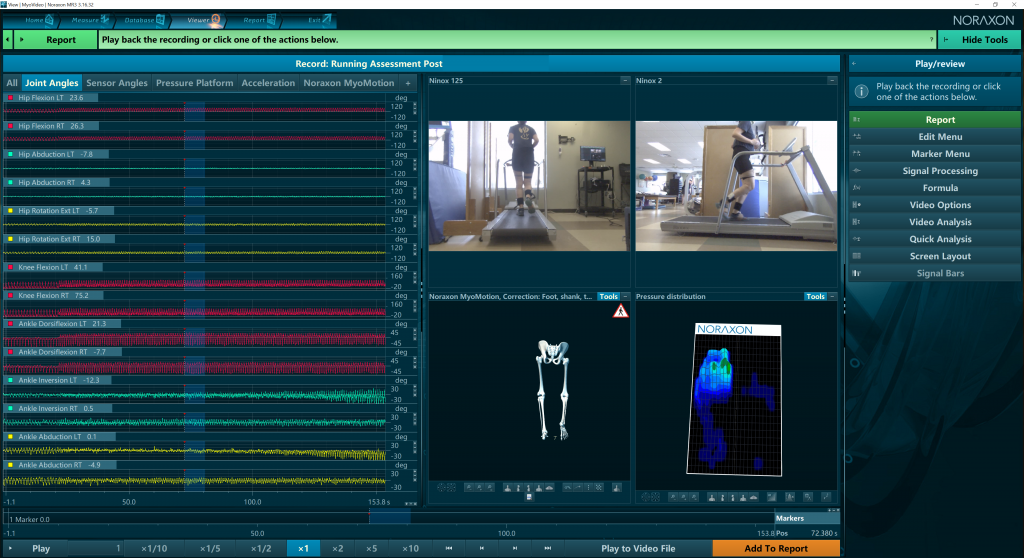
Portable Lab (lower body 3D Motion Capture, NiNOX 2D Video Cameras, Medilogic Pressure Insoles)
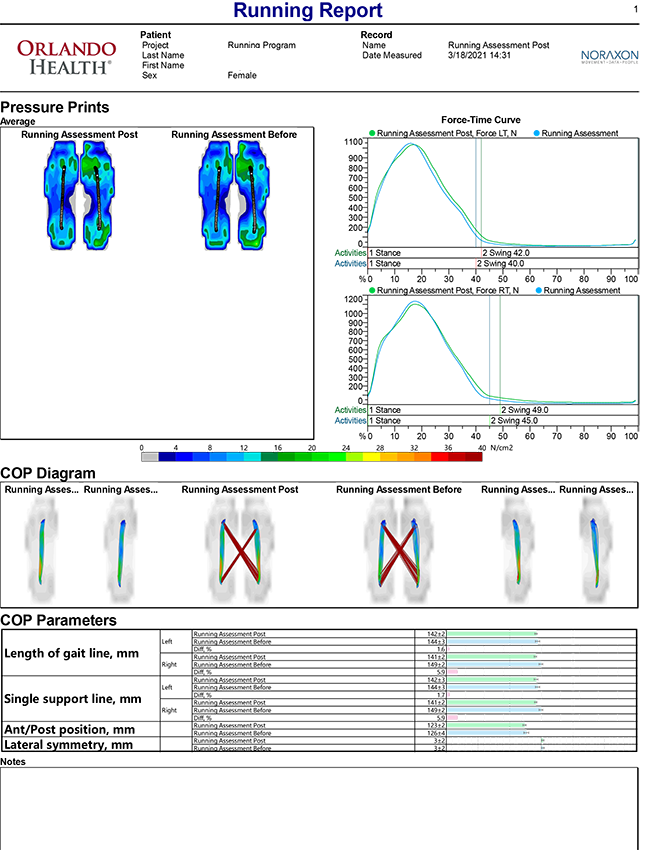
Key Improvements Shown in Comparison Report:
- Improved hip abduction angle by 55%
- Improved pelvic obliquity angle by 72%
- Reduction in lateral trunk lean
- Decrease in cross-over stride
Key Findings:
- Patient demonstrates crossover gait sign using video data. This lack of transverse/frontal plane control during stance phase is confirmed with motion data at the hip/pelvis during stance phase. Specific metrics that we looked at were hip IR, and pelvic rotation.
- Video data also reveals rigid, vertical trunk position. This most likely lead to “over striding”, and increased loading rate at initial contact. This was confirmed by the shallow knee flexion angle and decreased angle of inclination of the tibia at initial contact. Shallow knee flexion angle could also be indicative of eccentric quadriceps weakness.
- Patient demonstrates very low cadence with treadmill running. This combined with elevated loading rate and increased vertical displacement indicates the need for more efficient running mechanics.
Treatment summary:
- Based off of the physical examination, patient running mechanic deficits were primarily a result of poor strength and stability.
- Treatment started with building foundational strength through the lumbopelvic region and posterior lateral hip. Due to patient weakness, we started with table based exercises and progressed to more functional positions.
- Criteria to progress to next phase was no resting pain, satisfactory positioning with functional squat pattern and single leg stance.
- Once patient achieved this we worked in to more functional positions with the goal of mimicking stance phase as this is where patient demonstrates the most deficits. We used visual feedback, RNT training, and real time feedback with IMU to ensure patient was able to make appropriate neuromotor changes.
Assessment & Training Outcomes:
This client started off with 6/10 IT band pain with distance running and was able to run pain-free following treatment. The changes he made in the biomechanics of his pelvis and hips resulted in better stance vs. swing metrics with total contact duration decreasing by 5.1%. He also demonstrated an increased cadence from 166 to 174 steps per minute. This client was able to return to competitive distance running with improved mechanics and better performance.